Telnyx
AI voice agents for healthcare: use cases and ROI
See how teams deploy Voice AI Agents for intake, triage, scheduling, meds, and follow-up with HIPAA security and EHR integration.

AI voice agents for healthcare: use cases and ROI

Healthcare contact centers face a familiar challenge: patient demand grows faster than staffing budgets. Frontline staff are already stretched thin..
The issue isn’t just volume, it’s repetition. Front-desk teams ask the same intake questions. Nurses manage routine symptom calls. Physicians manually document information that could be automated.
Voice AI agents offer a path forward. They are built to handle these high-volume, repeatable conversations at scale. They automate intake, scheduling, symptom routing, and follow-up tasks, all while maintaining compliance. Some even support real-time documentation, turning spoken interactions into structured EHR notes on the spot.
The global AI voice agents healthcare market is projected to grow at a 37.79% CAGR from 2025 to 2030, reaching $3.175 billion by 2030.
Investing in the right platform requires careful evaluation of security architecture, workflow integration, and measurable outcomes.
This guide walks through the common use cases, technical requirements, implementation steps, and ROI metrics healthcare organizations need to de-risk a voice AI pilot.
Five use cases for voice AI agents in healthcare
Voice AI agents work best when they handle high-volume, structured conversations that follow predictable patterns. Here are five proven applications where voice AI agents deliver measurable value for healthcare right away:
Patient intake and registration
Voice agents can handle the first step of every patient interaction: intake. They collect demographic details, insurance info, and medical history before the appointment through a guided, spoken conversation.
As patients respond, the agent validates formats like date of birth or policy number, flags missing data, and submits everything directly to the EHR in real time. If there’s an issue, it routes the call to a human agent with full context intact.
Why it matters:
Front-desk staff spend hours a day repeating intake scripts. Offloading this process means faster check-ins, fewer errors, and better-prepared visits.
Symptom triage and care navigation
When a patient calls with symptoms, an AI agent can walk them through structured triage questions using clinical decision trees to assess severity. If symptoms suggest a minor issue, it may recommend home care. If urgent, it escalates to a nurse line or books the next available visit.
These assessments happen in real time with no need to wait for callbacks or manual note review.
Why it matters:
Licensed clinicians reviewing over 300,000 simulated interactions found voice agents delivered 99% accuracy in symptom triage with no instances of potentially severe harm. Standardized protocols reduce risk, and automation shortens wait times for urgent cases.
Appointment scheduling and reminders
Voice agents can pull up provider availability, schedule visits based on location or specialty, and confirm appointments during the same call. They handle reschedules, cancellations, and waitlist slots without involving a staff member.
Agents also send automated reminders via voice, SMS, or email and update the schedule instantly if a patient confirms or cancels.
Why it matters:
Manual scheduling is time-consuming and error-prone. With a voice agent, patients get immediate answers, and staff get time back. Organizations using real-time scheduling AI have seen no-show rates drop.
Medication adherence and refill management
Voice agents check in with patients on their medication schedules, ask about missed doses or side effects, and process refill requests. If a patient reports a potential adverse reaction, the agent can escalate to clinical staff immediately during the call.
All interactions are logged to the patient’s chart in real time.
Why it matters:
Medication adherence is a key driver of outcomes for chronic conditions. Voice agents don’t replace pharmacists, but they can flag early signs of risk and take routine refill follow-ups off staff workloads.
Chronic care follow-up and monitoring
Chronic care teams often manage large panels of patients who require ongoing support between visits. Voice AI agents can handle routine follow ups, ask about changes in condition, and escalate red flags directly to clinical staff in real time.
For example, if a patient with heart failure mentions sudden weight gain or shortness of breath, the agent can alert a care coordinator immediately. It can also document the interaction directly into the EHR and trigger follow-up workflows.
Why it matters:
Chronic care programs depend on timely intervention, but staff can’t field every call. Voice AI helps identify which patients need attention now and routes them accordingly, reducing the risk of readmissions and improving care continuity.
| Use case | Volume potential | Implementation complexity | Typical ROI timeline | Best for |
|---|---|---|---|---|
| Patient intake | High | Low | 3-6 months | Health systems with high appointment volume |
| Symptom triage | Medium-high | Medium | 6-9 months | Organizations with nurse lines or after-hours needs |
| Appointment scheduling | Very high | Low | 3-6 months | Any practice with scheduling bottlenecks |
| Medication adherence | Medium | Medium | 9-12 months | Chronic care programs, specialty pharmacies |
| Chronic care monitoring | Medium | High | 12+ months | Value-based care organizations, ACOs |
Multilingual and accessibility support
Healthcare organizations serve increasingly diverse patient populations. Language barriers and accessibility challenges can delay care, reduce satisfaction, and create compliance risks under civil rights requirements.
Voice AI agents can address these gaps by supporting:
- Real-time multilingual conversations to engage patients in their preferred language without relying on interpreter scheduling or third-party services
- Speech-to-text transcription to assist patients with hearing impairments by providing written summaries of voice interactions
- Adjustable pacing and repetition to accommodate elderly patients or those who need information repeated without frustrating wait times
- Dialect and accent recognition to improve comprehension across regional variations and reduce misunderstandings during intake or triage
For health systems serving LEP (Limited English Proficiency) populations, multilingual voice agents can expand access without proportionally increasing bilingual staffing costs. When evaluating platforms, ask which languages are supported natively, how new languages are added, and whether the system maintains clinical accuracy across translations.
Building voice AI with accessibility in mind is not just good practice. It ensures equitable care delivery and reduces risk of discrimination claims under Section 1557 of the ACA.
What to look for before deploying voice AI in healthcare
Automating high-volume tasks with voice AI can reduce workload, improve access, and speed up care. But getting it right requires more than conversation design. The platform itself needs to meet strict healthcare requirements for security, privacy, and reliability.Here’s what to evaluate before you move forward with any deployment.
HIPAA compliance and data residency requirements
Healthcare organizations must protect Protected Health Information (PHI) throughout the voice agent lifecycle. This means evaluating vendor architecture at multiple layers:
HIPAA-ready infrastructure
Look for platforms that sign Business Associate Agreements (BAAs) and maintain documented compliance programs. The infrastructure should include:
- Encrypted data transmission (TLS 1.2 or higher)
- Encrypted data storage with customer-managed keys
- Access controls with multi-factor authentication
- Audit logging for all PHI access
- Incident response procedures
HIPAA compliance isn't a feature you bolt on later. It requires purpose-built infrastructure designed with healthcare regulations in mind from day one.
Regional GPU deployment and data locality
Voice AI processing requires GPU compute, but not all platforms keep PHI within required geographic boundaries. Regional GPU deployment means conversation data stays in specific jurisdictions to meet state-level requirements or international regulations like GDPR.
Ask vendors: Where are your GPU clusters located? Can you guarantee that voice data and transcripts never leave a specified region? What happens during failover scenarios?
Telnyx deploys GPUs regionally alongside telephony Points of Presence (PoPs), so voice data processing happens close to the source without cross-border transfers.
Private network architecture
Public internet routing introduces security and quality risks. Private IP networks keep voice traffic off the open internet, reducing attack surface and improving call quality through dedicated infrastructure.
A private network architecture means:
- Voice packets travel through carrier-grade infrastructure
- No exposure to public internet threats
- Predictable latency and jitter
- Enhanced DDoS protection
When evaluating vendors, ask about their network topology and whether voice traffic ever touches public internet routes.
EHR integration and workflow automation
Voice agents deliver the most value when they connect directly to existing systems. Integration complexity varies by EHR platform and organizational IT policies.
Real-time API connectivity
Modern EHR platforms expose APIs for scheduling, patient demographics, clinical notes, and orders. Voice agents should authenticate securely and trigger API calls during live conversations, not batch-process data hours later.
Real-time integration enables:
- Live appointment availability during scheduling calls
- Insurance verification before booking
- Immediate note documentation in patient charts
- Medication history lookup during refill requests
Telnyx Voice AI Agents include real-time tool calling capabilities that invoke EHR APIs mid-conversation, so patients receive accurate information without delays.
Clinical workflow triggers
Beyond data exchange, voice agents should initiate workflows based on conversation outcomes. If a patient describes chest pain during triage, the system should automatically page a provider and flag the chart for immediate review.
Look for platforms that support:
- Conditional logic based on conversation content
- Webhook notifications to external systems
- Priority routing for urgent cases
- Structured handoffs to human staff
Implementation steps for a successful pilot
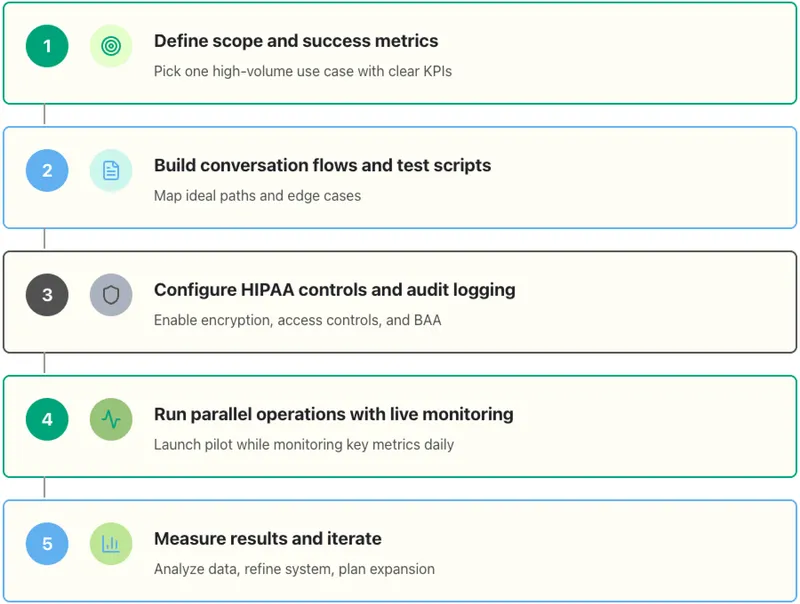
Most healthcare organizations start with a limited pilot before full deployment. Here's a phased approach that balances speed with risk management:
Define scope and success metrics
Pick one high-volume use case with clear success criteria. Appointment scheduling works well because it's easy to measure: call volume handled, scheduling accuracy, patient satisfaction, and staff time saved.
Set specific targets:
- Automate 60% of scheduling calls
- Maintain 95%+ booking accuracy
- Achieve 4.0+ patient satisfaction scores
- Reduce staff scheduling time by 30%
Build conversation flows and test scripts
Map out the ideal conversation path and all the likely branches. What questions will the agent ask? How should it handle interruptions or unclear responses? When should it escalate to a human?
Create test scripts covering:
- Happy path scenarios (everything works perfectly)
- Edge cases (unusual requests, unclear speech)
- Failure modes (system errors, unavailable data)
- Handoff scenarios (when to transfer to staff)
Configure HIPAA controls and audit logging
Before processing any real patient data, configure all security settings:
- Enable encryption for data in transit and at rest
- Set up access controls and authentication
- Configure audit logs to capture all PHI access
- Test incident response procedures
- Review and sign BAA with vendor
Run security testing and penetration tests before going live.
Run parallel operations with live monitoring
Launch the pilot while keeping existing processes intact. Run both systems in parallel so you can compare outcomes and catch issues before they affect patients.
Monitor key metrics daily:
- Call completion rate
- Escalation frequency
- Patient satisfaction scores
- System latency and reliability
- Staff feedback
Use the first two weeks to tune conversation flows, adjust escalation thresholds, and refine integration points.
Measure results and iterate
After 30 days, analyze pilot data against your success metrics. Where did the voice agent perform well? Where did it struggle? What surprised you?
Common learnings from healthcare pilots:
- Patients prefer voice agents for routine tasks but want human support for complex situations
- Clear escalation paths reduce patient frustration
- Integration reliability matters more than conversation sophistication
- Staff adoption requires training and trust-building
Use these insights to refine the system before expanding to additional use cases.
Vendor evaluation criteria
Not all voice AI platforms are built for healthcare's regulatory and operational requirements. Evaluate vendors across these dimensions:
Security and compliance foundation
- Do they sign BAAs?
- Are they SOC 2 Type II certified?
- Do they maintain HIPAA compliance documentation?
- Where are their data centers located?
- Can they support data residency requirements?
Voice quality and latency
- What's their average response latency?
- Do they co-locate GPUs with telephony infrastructure?
- How do they handle poor network conditions?
- What's their uptime SLA?
- How does audio quality compare in testing?
Organizations using accurate voice AI save customers 50–60% of correction time, so quality directly impacts efficiency.
Integration capabilities
- Do they offer pre-built EHR connectors?
- Can they support both HL7 and FHIR?
- Do they enable real-time API calls during conversations?
- What's their typical integration timeline?
- How do they handle version updates and API changes?
Pricing transparency and total cost
Voice AI pricing varies widely. Some vendors charge per minute, others per interaction or per agent seat. Hidden fees for transcription, storage, or API calls can significantly increase costs.
Telnyx offers transparent pricing at $0.06 per minute with end-to-end ownership of the voice stack, no markup on underlying telephony costs.
Compare total cost scenarios:
- Per-minute charges
- Setup and integration fees
- Ongoing maintenance costs
- Overage charges for high-volume periods
- API usage fees
Support and partnership approach
Healthcare implementations require ongoing support. Evaluate vendor responsiveness during the sales process. It's a preview of what you'll experience post-launch.
Look for:
- Dedicated technical account managers
- Clinical workflow expertise (do they understand healthcare operations?)
- Training resources for staff
- Regular product updates and feature releases
- Active user community or customer advisory board
Calculating ROI for voice AI agents
The value doesn’t stop at workflow efficiency. Voice AI investments need to demonstrate clear returns. Healthcare CFOs care about three areas: direct cost savings, revenue improvements, and risk reduction. Here’s how to evaluate ROI across these areas:
Direct cost savings
Calculate the fully loaded cost per call handled by staff versus voice AI. Include wages, benefits, training, management overhead, and facilities.
Example calculation:
- Current cost per call: $8.50 (average 6-minute call, $85/hour fully loaded cost)
- Voice AI cost per call with Telnyx: $0.09 per minute, or roughly $0.54 for a 6-minute call. (calculate here)
- Calls automated per month: 10,000
- Monthly savings = 10,000 × ($8.50 - $0.54) = $79,600
Call centers report 48% efficiency boosts with voice AI, with customer service costs dropping by 36%.
Revenue improvements
Voice agents increase revenue by:
- Reducing no-show rates through reliable automated, multi-channel reminders
- Capturing more appointments during peak calling hours
- Improving patient satisfaction and retention
- Expanding access to after-hours scheduling
Calculate the revenue impact of a five-percentage-point reduction in no-show rates multiplied by average appointment value and annual appointment volume.
Risk reduction and compliance
Quantifying risk reduction is harder, but consider:
- Reduced HIPAA violation risk from consistent security controls
- Lower malpractice exposure from standardized triage protocols
- Decreased staff burnout and turnover (replacement costs average 50-200% of salary)
Payback period
Most healthcare organizations see payback within six to 12 months for high-volume use cases like scheduling and triage. More complex applications like chronic care management may take longer but deliver compounding benefits over time.
Why Telnyx for healthcare voice AI agents
Telnyx supports healthcare organizations looking to automate high-volume conversations while staying compliant, connected, and in control.
We combine real-time voice AI capabilities with secure infrastructure to support the use cases that deliver the highest return, like patient intake, scheduling, symptom triage, and medication reminders. Our platform helps reduce operating costs, streamline staff workloads, and improve patient access without sacrificing accuracy or safety.
With:
- A HIPAA-ready voice AI stack and signed BAAs
- Regional GPU deployment for data locality
- Private network routing
- Seamless EHR integration
- Cost efficient transparent pricing
- End-to-end control of telephony, infrastructure, and AI
Telnyx helps healthcare teams move from pilot to proven ROI without unpredictable fees.
Start your healthcare voice AI pilot
In 2024, 43% of U.S. medical groups reported adding or expanding AI tools, up from 21% in 2023. Early adopters are establishing operational advantages that will compound over time.
Whether you're looking to reduce no-show rates, automate routine calls, or increase scheduling capacity, voice AI can deliver measurable value within months.
Start small. Choose a high-volume use case. Track performance. Scale based on results.
Healthcare teams ready to evaluate voice AI agents should prioritize vendors offering HIPAA-ready infrastructure, regional data processing, EHR integration capabilities, and transparent pricing. The right platform balances automation with clinical safety, efficiency with patient satisfaction, and innovation with regulatory compliance.
Learn more about Telnyx healthcare voice AI solutions at telnyx.com/solutions/healthcare
Building AI voice agents for healthcare? Join our subreddit.
Share on Social
Jump to:
Five use cases for voice AI agents in healthcareMultilingual and accessibility supportWhat to look for before deploying voice AI in healthcareImplementation steps for a successful pilotVendor evaluation criteriaCalculating ROI for voice AI agentsWhy Telnyx for healthcare voice AI agentsStart your healthcare voice AI pilotSign up for emails of our latest articles and news
Related articles
